By Bobby Shum
One month into his placement, pharmacist Bobby Shum describes the vital role that pharmacists play in antimicrobial stewardship and public health, and the importance of patience in making lasting change.
Cambridge University Hospitals Trust (CUH) pharmacist Bobby Shum and Norfolk & Norwich University Hospital (NNUH) microbiologist Stuart Drazich-Taylor are mid-way through a three-month placement in Kampala. They’re working alongside Ugandan colleagues as part of the CGHP-supported Kampala-Cambridge health partnership that is tackling antimicrobial resistance and optimising prescribing practices to improve maternal and neonatal health. One month into the placement, Bobby describes the vital role that pharmacists play in antimicrobial stewardship and public health, and the importance of patience in making lasting change.

From left to right: Bobby Shum, Kawempe Hospital pharmacist Ronald Onegwa, and microbiologist Stuart Drazich-Taylor.
Anguished cries broke the silence of a national maternity hospital in the centre of Kampala, Uganda. The wailing from outside reached me on the third floor. Rushing outside, I found a distraught crowd gathering around a man and his children, their sobs echoing through the chaos. The beloved wife, a mother of four, had passed away.
Such heart-wrenching scenes are tragically common in developing nations. While maternal death happens on average every two minutes, 95% of these deaths occur in low and lower-middle-income countries (World Health Organization data, 2020).
The United Nations set up 17 sustainable development goals in 2015 and called for action by all countries around the globe to end poverty, protect the planet, and tackle inequalities. The Kampala-Cambridge partnership I’m involved in contributes directly to Goal 3: Ensure healthy lives and promote well-being for all at all ages. In particular, the project aims to curb the worldwide threat of antibiotic resistance and optimise prescribing practices to improve maternal and neonatal health in Kampala. Most leading causes of fatal maternal complications, such as infections, are preventable and manageable.
I joined the partnership because I firmly believe in the pivotal role pharmacists can play in public health. By collaborating with other healthcare professionals, we can make significant contributions and empower our counterparts worldwide to reach the goal together. The opportunity to promote healthy and fulfilling lives for all, regardless of geographical boundaries, genuinely excited me.
The importance of antimicrobial stewardship cannot be understated
Antimicrobial stewardship stands as a cornerstone activity within the project. Its efficacy has been demonstrated as a cost-effective measure in slowing the progression of antibiotic resistance and reducing hospital-acquired infections. In the UK, pharmacists occupy a central role in antimicrobial stewardship. Equipped with comprehensive medication knowledge, they offer professional pharmaceutical advice to other healthcare professionals regarding appropriate antibiotic prescribing and monitoring. For instance, pharmacists assess antimicrobial prescriptions 48–72 hours post-administration, commonly referred to as antibiotic time-out, to evaluate the patient’s response and de-escalate the administration if appropriate. Pharmacists also have a leadership role in antimicrobial use surveillance, another vital part of antimicrobial stewardship activities.
Why sensible antibiotic use is vital
My primary interest lies in clinical pharmacy and medication safety, both of which intersect with antimicrobial stewardship. One common misuse of antibiotics is the prolonged use of these medications after surgery or procedures. A driving factor for this is to compensate for infection prevention and control measures that might be lacking. However, antibiotics are by no means harmless. For example, antibiotics cannot distinguish between good and bad bacteria, which disrupts the intricate ecosystem of microbes in our body. Without careful use, antibiotics kill susceptible bacteria and encourage resistant bacteria to survive and multiply.
Antimicrobial resistance poses a significant threat to us and our future generations. The United Nations predicts that by 2050, drug-resistant diseases could lead to the deaths of 10 million people each year and force more people into extreme poverty. Sensible antibiotic use is therefore crucial for reducing overall usage and slowing down the development of antimicrobial resistance.

From my perspective, empowering local pharmacists to actively engage in antimicrobial stewardship is a crucial driving force for the project’s success.
The visit so far
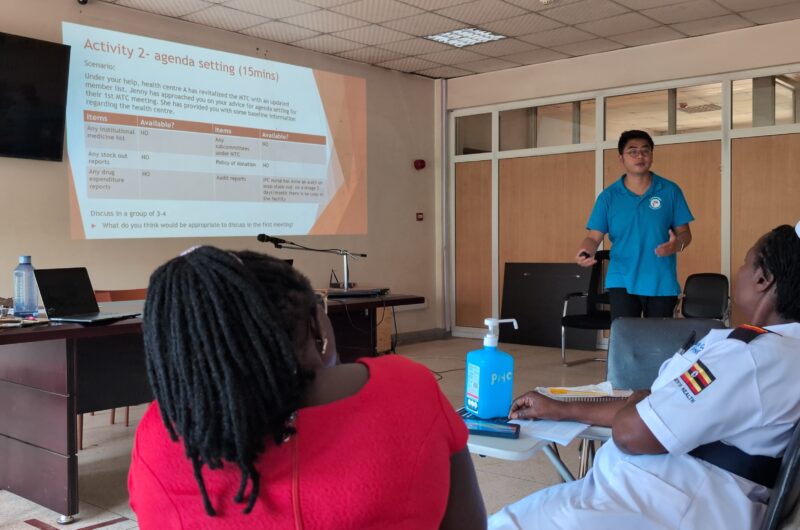
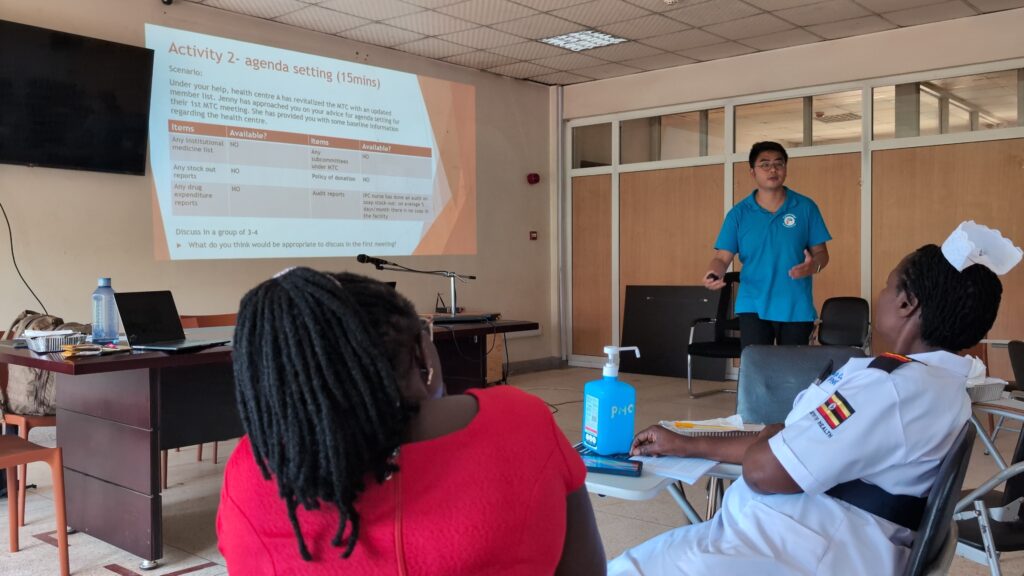
It has been a month since my arrival in Uganda, where one of my tasks is to foster sustainable local partnerships that are focused on healthcare empowerment. This means collaborating with local champions to develop an action plan for improving the antibiotic use process. I’m prioritising education on antimicrobial stewardship as well as nurturing the skills of local pharmacists to help ensure local communities receive high-quality and responsible healthcare services.
Pharmacist colleagues in Uganda are still in the developmental stages of expanding their pharmacy services. Currently, their responsibility has a heavy emphasis on supply chain management. From my perspective, empowering local pharmacists to actively engage in antimicrobial stewardship is a crucial driving force for the project’s success. Spending time with pharmacy interns and pharmacists in Kampala, I am impressed by their enthusiasm for clinical pharmacy and their dedication to embracing a broader role in patient care.
‘Patience wins battles’
One valuable lesson I’ve learned is the importance of patience and celebrating every success. To ensure a sustainable and lasting positive impact, it is crucial to keep everyone motivated and persistent. Stuart and I have encountered challenges in maintaining the momentum of the project, but have learned how to keep ourselves motivated and highlight the progress we’ve made. This experience has been instrumental in developing my leadership skills.
The team I work with is truly inspirational. Despite being busy with their various roles, they make time for quality improvement activities to enhance patient outcomes. For instance, they periodically collect antimicrobial use data to evaluate prescribing practices. To support them, we engage in collaborative activities and visit sites, fostering a learning and improvement culture. Their dedication to improving healthcare practices demonstrates their commitment to providing the best possible care for patients.
Outside of work, I’ve been on weekend adventures with my colleagues, enjoying the beauty of nature in national parks. From birds and reptiles to giant mammals like elephants, the diversity of wildlife leaves us spellbound. These experiences are adding lasting memories to this overseas placement.


Find out more about the Kampala-Cambridge AMS partnership.
If you are interested in supporting CGHP, please follow the donate button below or contact the team.
Return to blogs